You are viewing 1 of your 1 free articles
Easing the burden on the NHS
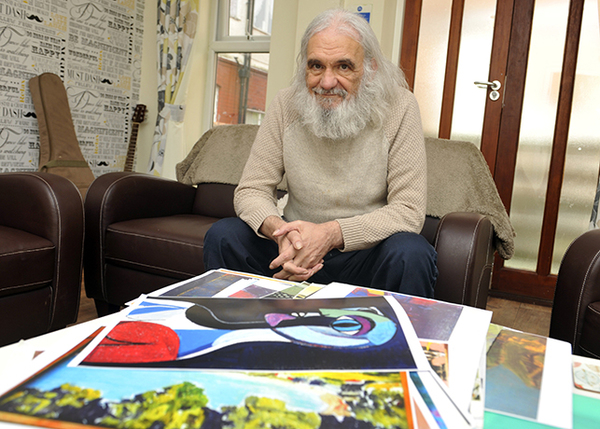
Housing association Home Group has hired medical practitioners to support its vulnerable tenants and ease the pressure on the health service. Tim Clark shadows its head of clinical practice for the day to find out how it’s working. Photography by Tim Clark
Dr Nichola Stefanou (left) and Fiona Ramsay outside Hawthorn House
Dr Nichola Stefanou is showing Inside Housing around the open plan office of her employer, Home Group, at its Newcastle headquarters. She points to an ordinary chair and, raising an eyebrow, she says: “Look, that’s where the chief executive sits. With everyone else! You wouldn’t get that in a hospital – they would have their own room.”
Dr Stefanou has an unusual role: a podiatrist who works for a housing association. But, if the sector’s plans to get more involved in healthcare come off, doctors may soon be commonplace on housing staff.
We’re spending the day with Dr Stefanou to get an insight into the sort of work that social landlords across the country may soon be doing.
Dr Stefanou started as Home Group’s head of clinical practice a year ago, fronting a six-strong team of healthcare professionals.
Our visit comes as hospital bosses admit that they have simply “run out of beds” and as the national news reports on patients dying in corridors. The crisis puts Home Group’s main strategic aim – to help reduce the burden of admissions into acute care – sharply into focus.
To start the day, we jump in a car and head to Cruddas Park, west of Newcastle’s city centre. We’re going to Hawthorn House, a grand Victorian mansion, which has been repurposed to house vulnerable adults.
The house is quiet enough to hear a pin drop and the refurbishment has built safety and security into the fabric of the home. All doors leading to rooms, for example, are secured with fingerprint access points.
The nine-bed service provides support to men who are at risk of homelessness or are homeless, most of whom have mental health and substance misuse problems.
The facility is one of a number of services Home Group provides for vulnerable men and women across the city. The landlord is the lead contract holder of the Newcastle Partnership, which provides housing, health and well-being support for clients with mental health issues and complex needs.
Along with Dr Stefanou, we’re here to meet Fiona Ramsay, who joined Home Group in July as mental health clinical lead, and Sarah Anderson, senior client services manager, to discuss future options for the sites under her charge, including Railway Terrace in North Tyneside, which supports ex-offenders and those at risk of reoffending.
The frustrations of the services manager quickly come to the fore, with issues arising from communication with NHS trusts to support workers dealing with situations involving high levels of risk, such as substance misuse or aggressive behaviour.
Clients under Home Group’s care include those who have been victims of paedophilia, while another has come to Home Group after being found unconscious with cigarettes stubbed out on them. After discharge from the NHS, the ‘step-down’ service is designed to rehabilitate people and help them get back into the community.
Ms Anderson says: “We end up taking all of the clients who have high support needs, which includes those who are not diagnosed [with mental health issues] because of substance misuse.”
It becomes evident that, in certain circumstances, Home Group has stepped in when there was a line that emergency services would or could not cross, either due to a lack of resources or remit, or with patients who show aggression.
Training regime
The team discuss a new training regime – psychologically informed practice (PIP) – which they are devising to help non-clinical Home Group staff, such as housing officers, identify warning signs and behaviours.
The training is not on the scale of professional psychiatry, but as Ms Ramsay says: “If we can get staff to a level where they understand when someone is at the point where they could relapse, or are at a particularly vulnerable point, staff should be comfortable having a conversation about it.”
Dr Stefanou adds: “The lack of integration of services means people may have a house, but they could still be drinking or suffering from an addiction and without care they could end up back in hospital.
“We need to work on their transition back into the community.”
“We want our impact to be felt long term and to make sure this is a strategic change.”
The term ‘bed blocking’ rarely comes up, but the main aim of the clinical team is to help bring people out of acute care and free up space in hospitals.
We are told that the average cost of a night on an acute ward is £350 – or double that if it is out of the county.Rachael Byrne, executive director of new models of care at Home Group, says that the equivalent care would only cost the housing association two-thirds or half that figure.
It was Ms Byrne who spearheaded the set-up of the new clinical team, and she explains that it started in response to the changing needs of tenants. Home Group may house up to 5,000 people who are in need of mental health support during any given year, according to Ms Byrne.
Commenting on the formation of the new clinical team, Ms Byrne says: “We want our impact to be felt long term and to make sure this is a strategic change. We want to work with [people with] mental health [issues] and learning disabilities, because we believe it is core to our founding principles.
“We will get commissioned and paid for [the services] but we also felt we needed to make a statement – we have issues in society we need to respond to.”
Of course, delving into healthcare also comes with risks, and up to half of Dr Stefanou’s time is spent managing governance for current and new services that Home Group provides.
But the clinician remains undaunted and her work ethic is ingrained. She explains how she completed her PhD while pregnant, mainly for something to do: “Otherwise I’d have got bored for sure.”
Lindsay Courtney (left), clinical lead for reablement and intermediate care, speaks in a comms meeting
Dr Stefanou came into the housing sector from Gateshead NHS Foundation Trust, where she was head of clinical governance.
“In health we visit people in their homes but do nothing about [the homes]. We go into houses and know they’re not appropriate but then leave again. Here we can actually change things,” she explains.
Dr Stefanou’s infectious optimism has helped the team come together, which has only been fully staffed for around three months.
“We're crap at social media. We're trained not to go on it.”
However what most excites her is having an active role in Home Group’s plans. Her eyes widen as she describes how, using smart key technology, people or their loved ones can control who has access to which parts of their home, whether it be the postman or a doctor, and the transformation this could have on their care and safety.
Next on the agenda for the day is a comms meeting with Lindsay Courtney, an occupational therapist by profession whose role as clinical lead for reablement and intermediate care is to assist clients to live as independently as possible and provide support to those at risk of readmission.
They work through options of how to communicate the team’s work both internally and also on social media, or “face place” as Dr Stefanou calls it.
“We’re crap [at social media],” she says, bluntly. “[Healthcare professionals are] trained not to go on social media. We’re always worried about breaching confidentiality.”
Language is one issue to tackle, both in how the clinical team liaise with the rest of Home Group, and how to meld the worlds of healthcare, technology and housing together. During the day the acronyms come thick and fast: CCGs, CQCs, the LHA cap and BIM.
A key barrier holding back co-operation between the NHS and housing associations has been an understanding of each other’s sectors. “You can’t go up to a commissioner and talk about a [housing] product,” Dr Stefanou says. “They wouldn’t listen. You have to talk their language to get an understanding of how what we do can help them.”
The last appointment of the day is a visit to Northumbria University, where Lars Erik Holmquist, professor of innovation, describes the “trough of disillusionment”. The trough, along with the “peak of inflated expectation”, comes at the end of an hour-long working meeting to map out plans between the university and Home Group to spearhead new research into assistive technology.
It’s not every day you see a trained podiatrist listen intently to conversations about troughs, peaks or for that matter construction methods such as BIM, artificial intelligence and the downfalls of buying a smart fridge.
Yet Dr Stefanou cracks a smile, rubs her palms and without hesitation tells the professor: “I’m excited.”
In the car afterwards Dr Stefanou is still buoyed by the thrill of new possibilities that the role has opened up. “It’s a bit like that Tom Cruise film Minority Report, isn’t it?” she says. “But not as dramatic.”
UPDATE 17.1.18 4.55pm This article originally stated that Hawthorne House was part of the North Tyneside Recovery Partnership. It has also been updated to clarify that Sarah Anderson's comments refer to a project called Railway Terrace, which is part of the North Tyneside partnership.